|
|||
The contribution of neuroimaging to the improvement of the quality of life of patients suffering from epilepsy
VLAIKIDIS N.D.
A' Neurological Clinic of Aristotle University in Thessaloniki (Dir.: Prof. S. I. Baloyannis)
Summary
The epileptic seizures affect, because of different causes, all ages of (children - adults - aged) human beings. Although the seizures do not last more than a couple of minutes every few months or year, the patients describe significant worsening of their quality of life.
The Neuroimaging can disclose the lesion, which provokes the epileptic seizures and offers (always in connection to the clinic) the best help to the differential diagnosis of this lesion.
Epilepsy surgery can result in longterm improvement in seizure control and quality of life (QoL) in carefully selected patients with intractable tumorrelated epilepsy, temporal lobe epilepsy, even in tuberous sclerosis complex epilepsy cases.
Also in cases of functional electrostimulation with brain-stem implants, aiming for epilepsy control and restoration of locomotion and grasp faculties of the patient, Neuroimaging will decide on the points, where the implants should be put, as well as on the most appropriate and safe route of the approaching to this area, thereby reducing the incidence of postoperative neurological deficits and significantly improving the overall quality of life of the patients.
Key words: Epilepsy, Epileptic seizures, Quality of Life (QoL), Neuroimaging.
Introduction
The epileptic seizures affect, because of different causes, all ages of (children - adults - aged) human beings. Although the seizures do not last more than a couple of minutes every few months or year, the patients describe the worsening of their quality of life, because of difficulties in driving (64%), independence (54%), employment (51%), social embarrassment (36%), medication dependence (33%), mood/stress (32%), and safety (31%)1 or may otherwise be totally disabled2. Nowadays because of the great number of traffic accidents and the increasing number of patients with posttraumatic epilepsy, more and more people need to improve their quality of life3.
Neuroimaging findings
The main methods in the management of the epileptic patients are the clinical signs, the EEG (plain, after activation, with nasopharyngeal or sphenoidal electrodes, after 24hours video-monitoring, brain surface EEG) and the Neuroimaging (x-ray images, CT, MRI, fMRI, MRI-Spectroscopy, PET or SPECT).
The Validation of the Clinical Signs is often difficult because the events are brief, unexpected, rarely observed by competent observers, and rarely remembered adequately, if at all, by the patient. So if no tongue bite or urine loss exist, the clinical symptoms aren't efficient for the diagnosis of the epileptic seizures.
The EEG is the most important diagnostic method for epilepsy.
The proportion of abnormal EEG findings in patients with epilepsy varies according to the seizure type. Recordings performed with the patient asleep are more likely to reveal spike foci over the temporal lobe than are routine recordings. Nasopharyngeal electrodes are of greater value than sphenoidal electrodes for identifying temporal foci. Depth electroencephalography can reveal foci not apparent with surface recordings, or define them better, or indicate that an apparent single focus is multiple.
Topographical EEG mapping has, to date, not provided superior evidence of localization of focal epileptic discharges compared to conventional recordings.
However, many people have EEG abnormalities, which could be compatible with epilepsy without suffering from it. The Neuroimaging can help the declaration of the diagnosis of epilepsy in the ambiguous cases.
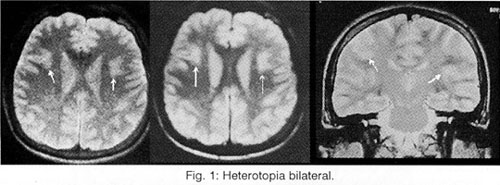
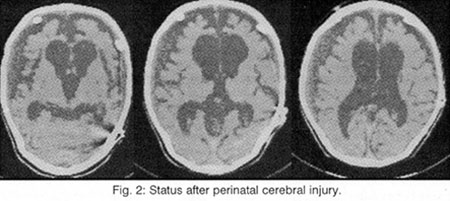
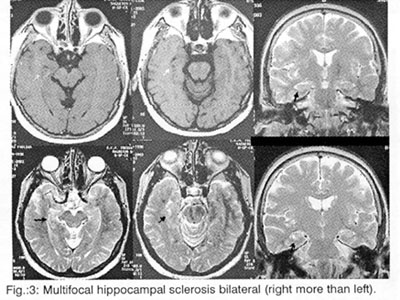
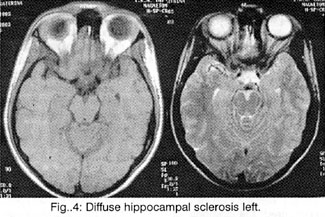
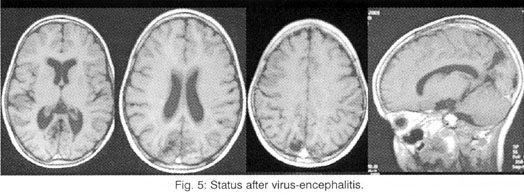
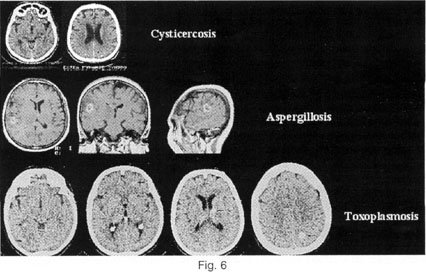
But the most important task of the Neuroimaging is (always in connection to the clinic) the help to the localisation of the lesions (which provoke the epileptic seizures), to the differential diagnosis of this lesion among hereditary illnesses (phacomatoses, leukodystrophies), abnormalities of development (dysplasias, vascular malformations, neuronal migration disorders: heterotopia-double cortex syndrome (Fig. 1), schizencephaly, lissencephaly, unilateral Megalencephaly), perinatal cerebral injuries (between the 30th week of pregnancy and the end of the first month of life due to placental insufficiency, hypoxia, infections, intoxication and mechanical birth trauma4, presented as porencephaly, focal or generalized enlargement of the ventricular system or the subarachnoid space (Fig. 2), hippocampal sclerosis (Fig. 3 and 4) or acquired lesions (benign or malign neoplasms, cerebrovascular diseases, encephalitis (Fig. 5), cerebral abscess, parasitic, fungal and protozoan diseases (Fig. 6), cerebrocranial injuries, degenerative diseases), for the best coping with the patient's problem (conventional pharmaceutical or neurosurgical treatment), as well as for the prognosis before and after the preferred therapy.
Discussion
Overall results showed that 62% of the patients experienced an outcome of "cure" or "almost cure", although the patients who experienced a significant reduction in seizures but who continued to have intractable epilepsy were not considered to have had a good result5.
The substantially increased risk of seizures and epilepsy in the elderly is associated with medical conditions that affect this group such as stroke, dementia, and metabolic disturbances. In addition, there is an increased incidence and associated mortality of status epilepticus among seniors6.
Patients with complete tumor resection and no interictal epileptiform activity on postoperative EEG studies had the best operative outcome. Epilepsy surgery can result in long-term improvement in seizure control and quality of life (QoL) of the selected patients with intractable tumor-related epilepsy7.
The recent advances in Neuroimaging with 3 Tesla MRI, fMRI and MRI-Spectroscopy, the Diffusion Tensor Imaging8, but also with PET and SPECT brought the possibility of a better diagnostic procedure and the help of the Neurosurgery in the management of epileptic cases.
Epilepsy surgery can result in long-term improvement in seizure control and quality of life (QoL) of the selected patients with intractable tumorrelated epilepsy9, temporal lobe epilepsy10 , even in tuberous sclerosis complex epilepsy cases11 and offers also improvement of quality of life of the whole patient's family.
Functional rehabilitation is an original task of neurosurgery from the very outset. Progress in the fields of microelectronics, computer technology, and genetic engineering along with rehabilitation science is opening up a new field of unknown chances. At present, the Functional Neurosurgery plays a major role in neurosurgical rehabilitation to partially restore lost body functions and to help improve the quality of life of disabled patients with functional electrostimulation, brain-stem implants, pain and epilepsy control, restoration of locomotion and grasp faculties3.
Also the classic epileptic neurosurgery can improve the QoL of the epileptic patients removing the pathological alterations and especially in the cases of temporal epilepsy either with en block temporal lobectomy (Falconer) or transcortical approach amygdaloippocampectomy (Niemeyer), pterional approach amygdaloippocampectomy (Yasargil), modified hemispherectomy or incision of the corpus callosum, the most important connection between the cerebral hemispheres in order to prevent the spread of the epileptic activity from one cerebral hemisphere to the other.
The Neuroimaging determines the area of the intervention, maps out the route of the approaching to this area and helps to the complete and safe resection of seizure foci, thereby reducing the incidence of postoperative neurological deficits and significantly improving the overall quality of life of the patients12.
Even the children with epilepsy due to tuberous sclerosis complex, which is frequently severe, drug-resistant often multicentric and may have a negative impact on the child's global development, may be candidates for epilepsy surgery, if it is possible to determine the leading epileptogenic tuber. Patients with tuberous sclerosis complex and drug-resistant epilepsy may benefit from epilepsy surgery with reduction in frequency and severity of seizures as well as improved mental and behavioural development leading to a better quality of life13.
Last but not least the Neuroimaging helps to confrontate the psychic burden from the epilepsy. Hippocrates noted in about 400 BC that: Melancholics ordinarily become epileptics, and epileptics melancholics: of these two states what determines direction is the direction the malady takes; if it bears upon the body, epilepsy, if upon the intelligence, melancholy14.
Depression is the most common comorbid condition associated with epilepsy, based on epidemiological studies, with prevalence in published studies ranging from 20 to 55% in patients with recurrent seizures and 3 to 9% in patients with controlled epilepsy15-18. Robertson reviewed 17 studies pertaining to mortality in epilepsy and summarized that suicide was nearly 10times more frequent than in the general population19.
Several studies have compared the findings on depression assessments with the results of Neuroimaging tests in patients with epilepsy. Most have found that lesions or functional abnormalities were associated with more severe symptoms of depression20,21.
Gilliam et al. also found a significant correlation between extent of 1H magnetic resonance (MR) spectroscopy abnormalities in the temporal lobes and Profile of Mood States scores20. None of these studies found an association between lateralization of the epileptogenic zone and depression.. Other groups have found increased metabolism in the left amygdala using 18F DG positron emission tomography (PET)22 A recent summary of neuroimaging and neuroanatomical studies of depression indicates that current data support a role for dysfunction of the prefrontal and striatal systems in the pathogenesis of depression23. Intriguing recent data suggest that some metabolic abnormalities can normalize after effective pharmacological or interpersonal therapies for depression24,25.
Multiple neurochemical, neuroanatomic, neuroendocrinologic, and functional neuroimaging efforts are attempting to establish a unified neurobiology of anxiety. These investigations have contributed to the synthesis of anxiety circuitry schematics such as that shown26.
As seen in the figure, central to the anxiety model of most theorists is the amygdala, hypothesized to be the key structure integrating interoceptive and exteroceptive stimuli, and distributing processed afferent data to the multiple efferent systems (cortical, limbic, basal ganglia, hypothalamic, brain stem) which produce the autonomic, affective, cognitive, and endocrinologic components of the anxiety response. Seizures, regardless of type and magnitude, represent an acute fundamental disruption to neuropsychiatric homeostasis, thereby necessarily impacting this circuitry27.
We studied recently 22 patients with anxiety and refractory epileptic seizures with a circulus vitiosus between these pathological states. The effective confrontation of anxiety controlled the epileptic seizures of these patients.
REFERENCES
- Gilliam F, Kuzniecky R, Faught E, Black L, Carpenter G, Schrodt R: Patientvalidated content of epilepsyspecific qualityof-life measurement. Epilepsia, 1997, Feb; 38:2336:Issue: 2
- Joynt RJ, Griggs RC: Clinical Neurology, 1997; Lippincott-Raven Publishers, Philladelphia - New York.
- von Wild KR. New development of functional neurorehabilitation in neurosurgery. Acta Neurochir Suppl, 2003; 87:43-7.
- Jellinger K:Spezielle Pathologie des zentralen und peripheren Nervensystems sowie neuromuskularen Peripherie. In: Holzner JH: Pathologie des Menschen, 1976, Urban und Schwarzenberg, Munchen.
- Keogan M, McMackin D, Peng S, Phillips J, Burke T, Murphy S, Farrell M, Staunton H: Temporal neocorticectomy in management of intractable epilepsy: long-term outcome and predictive factors. Epilepsia. 1992 Sep-Oct; 33(5):852-61.
- LaRoche SM, Helmers SL. Epilepsy in the elderly. Neurolog. 2003 Sep; 9(5):241-9.
- Britton JW, Cascino GD, Sharbrough FW, Kelly PJ: Low-grade glial neoplasms and intractable partial epilepsy: efficacy of surgical treatment. Epilepsia. 994 Nov-Dec; 35(6):1130-5.
- Bassam A. Assaf, Feroze B. Mohamed, Karine J. Abou-Khaled, J. Michael Williams, May S. Yazeji, John Haselgrove, and Scott H. Faro: Diffusion Tensor Imaging of the Hippocampal Formation in Temporal Lobe Epilepsy. AJNR Am J Neuroradiol 24:1857-1862, October 2003.
- Britton JW, Cascino GD, Sharbrough FW, Kelly PJ: Lowgrade glial neoplasms and intractable partial epilepsy: efficacy of surgical treatment. Epilepsia.1994 Nov-Dec; 35:11305: Issue:6
- Ryvlin P: Beyond pharmacotherapy: surgical management. Epilepsia, 2003; 44 Suppl 5:23-8.
- Karenfort M, Kruse B, Freitag H, Pannek H, Tuxhorn I: Epilepsy surgery outcome in children with focal epilepsy due to tuberous sclerosis complex. Neuropediatrics, 2002 Oct;33(5):255-61.
- Chabrerie A, Ozlen F, Nakajima S, Leventon ME, Atsumi H, Grimson E, Keeve E, Helmers S, Riviello J Jr, Holmes G, Duffy F, Jolesz F, Kikinis R, Black PM. Three-dimensional reconstruction and surgical navigation in pediatric epilepsy surgery. Pediatr Neurosurg, 1997 Dec; 27(6):304-10.
- Karenfort M, Kruse B, Freitag H, Pannek H, Tuxhorn I. Epilepsy surgery outcome in children with focal epilepsy due to tuberous sclerosis complex. Neuropediatrics. 2002 Oct; 33(5):255-61.
- Lewis AJ. Melancholia: a historical review. J Ment Sci 1934;80:1-42.
- Lambert MV, Robertson MM. Depression in epilepsy: etiology, phenomenology, and treatment. Epilepsia 1999; 40(Suppl 10):21-47.
- O' Donoghue MF, Goodridge DM, Redhead K, Sander JW, Duncan JS. Assessing the psychosocial consequences of epilepsy: a community-based study. Br J Gen Pract 1999;49:211-4.
- Jacoby A, Baker GA, Steen N, Potts P, Chadwick DW. The clinical course of epilepsy and its psychosocial correlates: Findings from a UK Community study. Epilepsia 1996; 37:148-61.
- Robertson MM, Trimble MR. Depressive illness in patients with epilepsy: a review. Epilepsia 1983; 24(suppl 2):S109-16.
- Robertson MM. Suicide, parasuicide, and epilepsy. In: Engel J, Pedley TA, editors. Epilepsy: a comprehensive textbook, 1997. Lippincott-Raven, Philadelphia.
- Quiske A, Helmstaedter C, Lux S, Elger CE. Depression in patients with temporal lobe epilepsy is related to mesial temporal sclerosis. Epilepsy Res 2000; 39:121-5.
- Schmitz EB, Moriarty J, Costa DC, Ring HA, Ell PJ, Trimble MR. Psychiatric pro.les and patterns of cerebral blood flow in focal epilepsy: interactions between depression, obsessionality, and perfusion related to the laterality of the epilepsy. J Neurol Neurosurg Psychiatry 1997;62:458-63.
- Drevets WC, Price JL, Bardgett ME, Riech T, Todd RD, Raichle ME. Glucose metabolism in the amygdala in depression: relationship to diagnostic subtype and plasma cortisol levels. Pharmacol Biochem Behav 2002;71:431-47.
- Drevets WC. Neuroimaging and neuropathological studies of
depression: implications for the cognitive-emotional features
of mood disorders. Curr Opin Neurobiol 2001;11:240-9. - Brody AL, Saxena S, Stoessel P, et al. Regional brain metabolic changes in patients with major depression treated with either paroxetine or interpersonal therapy: preliminary findings. Arch Gen Psychiatry 2001;58:631-40.
- Brody AL, Saxena S, Mandelkern MA, Fairbanks LA, Ho ML, Baxter LR. Brain metabolic changes associated with symptom factor improvement in major depressive disorder. Biol Psychiatry 2001;50:171-8.
- Davis M. Functional neuroanatomy of anxiety and fear: a focus on the amygdala. In: Charney DS, Nestler EJ, Bunney BS (eds). Neurobiology of mental illness. New York: Oxford Univ Press, 1999: 463-74.
- Goldstein MA, Harden CL: Epilepsy and Anxiety. Epilepsy & Behavior, 2000 (1): 228-34.
